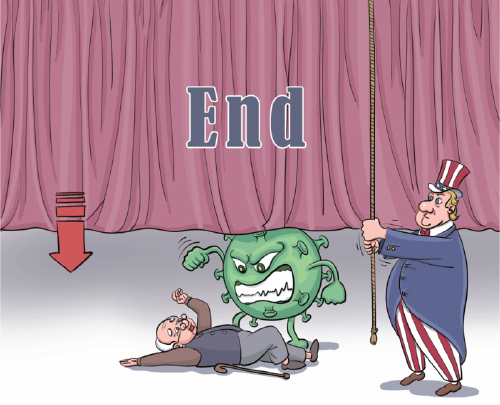
Virus is still winning in the US
Once again, COVID-19 is rampaging unchecked through the US population, because there are no longer any public health measures in place to protect adequately against infection. I myself have taken extraordinary precautions to avoid infection for the last two and a half years, because I met three of the qualifications for severe COVID-19: I am 77 years old; I am a cancer survivor; and for the past 40 years I have been treated for a chronic inflammatory condition that leaves me moderately immunocompromised.
Luckily, I had the privilege of being able to sequester myself in my country home, where I could limit my personal interactions. I was vaccinated within weeks of vaccines becoming available, and I have received boosters every three to four months since. Moreover, I was given Evusheld, a monoclonal antibody treatment, four weeks ago.
Yet, toward the end of May, after many months of seclusion, I permitted myself one social occasion-a fundraising event with about 100 people in attendance. Four days later, in bed with a fever, cough and malaise, I tested positive for COVID-19. Even with multiple vaccinations and Evusheld, I was not protected.
My experience has underscored a sad truth. In the race to return to some semblance of normalcy, the needs of the vulnerable have been forgotten.
Given that infection by SARS-CoV-2, the virus that causes COVID-19, has now become almost inevitable for most people, the least we could do is develop drug treatments to alleviate disease symptoms and prevent death and long-term consequences. But we have not done so. Pharmaceutical companies designed and manufactured COVID-19 vaccines on an unprecedentedly accelerated timeline, but drug development has not proceeded apace.
There are three main treatment options for those who develop COVID-19 and are at risk of long-term effects and disability. All three have limitations that prevent wider use. The first is remdesivir, which requires an intravenous-administered infusion and is thus available only in clinical settings.
The second is Evusheld, which its developer, AstraZeneca, claims is effective in preventing infection from the latest Omicron subvariants of the novel coronavirus. However, in my case at least, the treatment failed to work as it should.
The third is Paxlovid, an antiviral drug developed by Pfizer that targets the SARS-CoV-2 protease. Paxlovid gained popularity as a COVID-19 treatment when studies showed that it reduced the risk of serious illness and death by up to 90 percent. But research into its prophylactic potential has turned up empty, and new evidence suggests that some who take it experience rebound infections, meaning they might unwittingly transmit the virus to others.
What is to be done? Since the start of the pandemic, I have argued that vaccination alone will not be enough to prevent repeated COVID-19 infections. The literature on cold-causing coronaviruses shows that they can reappear like clockwork. And with SARS-CoV-2, waves of infection occur not annually, as I would have expected based on previous data, but rather at much shorter intervals-every four to six months.
In addition to recognizing the limitations of vaccination as a form of pandemic control, we are becoming more aware of the seriousness of "long COVID," which has a broad range of symptoms-respiratory, gastrointestinal, neurological-that persist after an initial COVID-19 infection has cleared.
While more than one-third of COVID-19 patients will develop long-term symptoms of some kind, 2-4 percent will experience consequences severe enough to be disabling for many months, if not years. These include intense fatigue, persistent pain and damage to vital organs, such as the heart, lungs, pancreas, and possibly others. Millions of people around the world have "long COVID", and millions more will end up with it. Recent data suggest that the vaccines reduce its impact by a mere 15 percent.
While our path out of the pandemic is not as straightforward as when I was working as an HIV researcher, the overarching direction of travel is still clear. We must develop strong antiviral drugs specifically targeted at SARS-CoV-2. Though only six drugs targeting HIV have been identified, we have several treatments that are effective at clearing the virus.
Given the technological advances made in the last 30-35 years, and the speed with which these advances led to a COVID-19 vaccine, I had expected that we would have numerous antivirals for COVID-19 by now. And yet, of the treatments that have been approved, all are retreads or drugs developed for other viruses, not SARS-CoV-2.
What we need now is to repeat the approach that worked during the HIV/AIDS epidemic. That effort involved a multi-year drug-development program to guide government- and industry-sponsored research. As a member of the National Institute of Allergy and Infectious Diseases Council, I proposed an intensive, cooperative program whereby universities with industrial partners would receive large grants to fund basic research and practical drug development. The potential for a payoff attracted the interest of large pharmaceutical and biotechnology companies and spurred the formation of several public-private partnerships.
The program was a resounding success, but it didn't come cheap. Each year, the National Institutes of Health set aside $2-3 billion in a special HIV/AIDS research budget. The same level of investment is needed again. My colleagues around the world who have the skills required for intensive COVID-19 research are desperate for additional funding.
To its credit, the NIH recently awarded $108 million in grants to the Metropolitan AntiViral Drug Accelerator, a collaborative initiative by world-class research institutions in New Jersey and New York that will investigate the potential for small-molecule drugs to treat and prevent coronaviruses. Combinations of small-molecule antiviral drugs have proved effective in preventing and treating HIV, and can be manufactured and sold cost-effectively. A year's treatment with HIV drugs now costs well under $100 in many places around the world. A protocol to prevent and treat COVID-19, lasting two to three weeks at most, should cost far less.
Unless we find powerful ways to eliminate the SARS-CoV-2, it will remain a scourge. Some strains are only a mutation or two away from a leap in lethality. To prevent that, we must learn from pandemics past.
Project Syndicate
The views don't necessarily reflect those of China Daily.
The author, a scientist, biotech entrepreneur, and infectious disease expert, is chair and president of the global health think tank ACCESS Health International.
If you have a specific expertise, or would like to share your thought about our stories, then send us your writings at opinion@chinadaily.com.cn, and comment@chinadaily.com.cn.


































